Ward Clerks

What they do
They are the friendly face that you will likely see first when you enter the ward during the day. They will check with you your contact number, address and other details when you are first being admitted into the ward. The Ward Clerk will also show you to your room.
The Ward Clerk will assist you with any enquiries you may have and pass on messages that come into the ward for you. They can also help with notifying other staff on the ward that you require assistance.
Ward Clerks are happy to help when the need arises and enjoy the opportunity if you ever want a friendly chat, too.
When you may see them
The Ward Clerk might come to your room with messages about appointments.
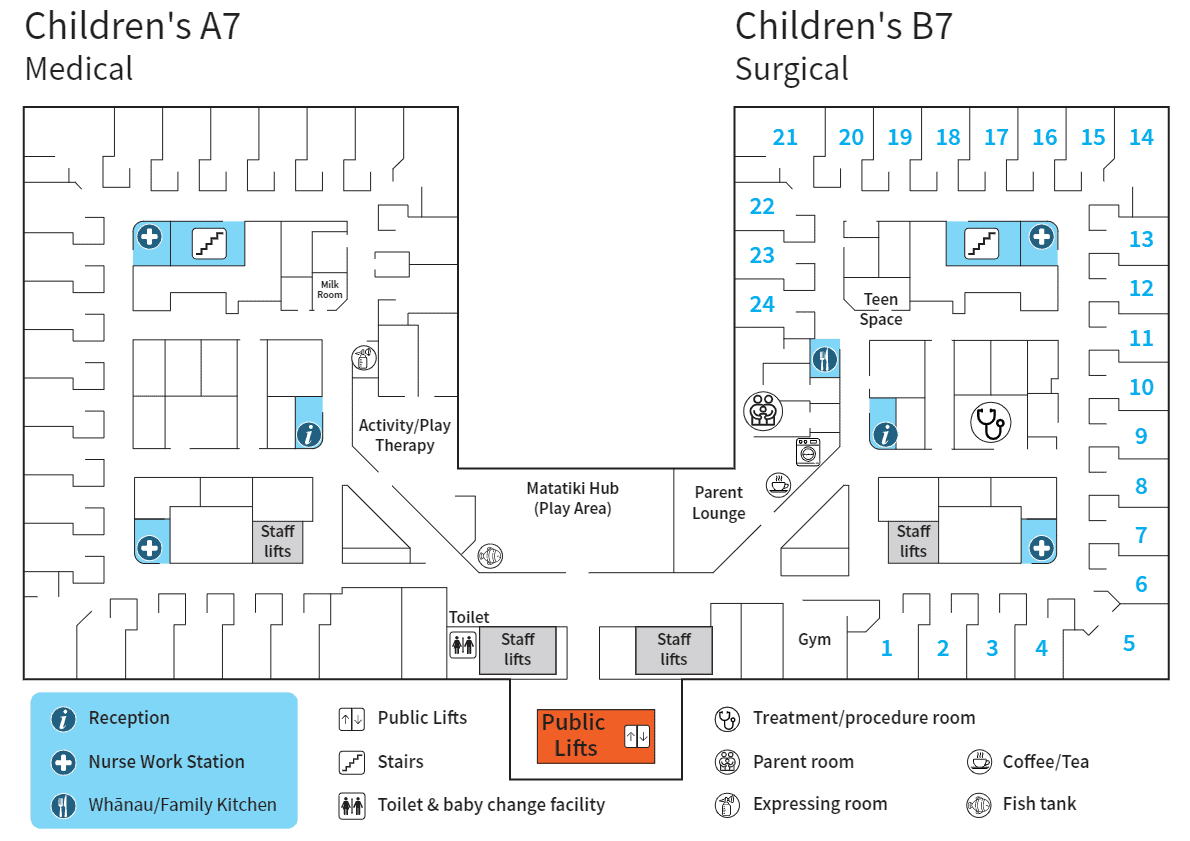
They can help you find your way around the ward.
You can give them money for parent meals you may order.
Charge Nurse Manager

What they do
They are responsible for overseeing the nursing staff and the care they give. They are also responsible for the overall running of the ward. The Charge Nurse Manager will know about you and your child even if you don’t see us during your stay. They will be involved with multidisciplinary team meetings and decisions about your child.
When you may see them
You can ask to see us if you would like to talk about the care your child is getting. You might want to give us feedback about your stay in hospital or about a member of staff.
Social Workers

What they do
Child Health Social Workers are Registered Social Workers employed by the CDHB to help and support children and their families who are patients of the Paediatric Service at Christchurch Hospital.
When you may see them
Child Health Social Workers are committed to Bi-Cultural Practice in accordance with the Principles of the Treaty of Waitangi and offer support and assistance in areas such as new diagnoses, trauma, chronic conditions impacting on families, care and protection of children, advocacy, and connecting families to community and social supports.
If you would like to talk with a Child Health Social Worker please discuss this with your child’s nurse and/or medical team.
Occupational Therapists

What they do
Occupational Therapists help children and their whanau to be as safe & independent as possible with activities they do every day.
When you may see them
This may include toileting, showering, dressing, playing, eating and managing tiredness & routines; maximising how children’s’ brains and bodies work.
Physiotherapists

What they do
Physiotherapists help babies and children who have a variety of different injuries or illnesses to improve their movement and function through play, exercise, education and advice.
Cleaners

What they do
The cleaner is responsible for cleaning the ward, bedrooms, bathrooms, dusting, rubbish, vacuuming, wet mopping, replenishing supplies, paper towels, soaps, toilet rolls, removing marks off walls etc.
When you may see them
Parents and children will see a cleaner anytime Monday to Sunday anytime from 6:30-8am start.
Hospital Play Specialists

What they do
Hospital Play Specialists are paediatric healthcare professionals who work with children and families in hospital to help them cope with the challenges of hospitalisation, illness and disability. Their role helps improve patient and family care, satisfaction, and overall experience.
Infants, children and youth confront a wide variety of stressful and potentially traumatic events that can impact their ability to cope in a hospital admission. These experiences related to healthcare can lead to feelings of fear, confusion, loss of control and isolation that can inhibit their development and have negative effects on their physical and emotional health and well-being. Hospital Play Specialists will assess the child’s needs alongside the family and other medical staff, then support and make a plan to get the most desirable outcome.
When you may see them
A child or parent can be referred to a Hospital Play Specialist by any member of a multi-disciplinary medical team or parent specifically in the Paediatric Wards but not limited to other areas within the hospital. They will provide children with age-appropriate preparation for medical procedures, oral medicine taking difficulties, pain management and coping strategies, and play and self-expression activities.
They also provide information, support, and guidance to parents, siblings, and other family members.
We have an Activity Room situated in A7 for all Paediatric inpatients (Both A7 and B7 inpatients) which is licensed by the Ministry of Education as a Hospital Based Education and Care Service. We are regularly reviewed by the Education Review Office and are guided by the Early Childhood Curriculum Te Whāriki. We are staffed by qualified, registered Early Childhood Teachers. This space is a place which is free from medical interventions where children can play; engage, interact with others, express their emotions, make sense of what is happening for them and most importantly have fun.
Hospital Play Specialists also see children in the Paediatric Outpatient ward to support them for blood tests and other non-admission procedures. Paediatric Outpatient Staff will make a referral to assist children in this area.
Maori Health Service

What they do
Ko tā te Whānau o Hauora Māori, he manaaki i ngā tūroro me ā rātou whānau kia māmā ake te whakamātūtū a te tūroro. E ngana ana te whānau o Hauora Māori ki te tūtaki i ngā tūroro o te hōhipera. He pai noa hoki te tono mo tētahi kaiāwhina hei tautoko i a koe. Mā ngā nēhi to puka e tukuna, rānei waea atu ki te kaimahi Hauora Māori 027 458 0095.
The Māori Health team work closely with patients and their whānau to better navigate the health care system. The Māori Health team attempt to meet all Māori patients admitted to the hospital, however if you feel that you would like the support of Māori Health throughout your admission, referrals can be made through the nursing staff. Alternatively, you can contact the paediatric Māori Health worker on 027 458 0095.
Pharmacy
What they do
Paediatric pharmacists are part of the wider multi-disciplinary team who care for all children admitted to hospital or in the outpatient clinics. Ultimately they’re responsible for the provision of appropriate medicines for the patients and act as ‘drug detectives’ to ensure that the medications that are charted for the child are appropriate for their clinical condition.
When you may see them
Patients and families can most frequently spot the paediatric pharmacists in their natural habitat on the ward. They’re most likely to encounter the pharmacist when they’re first admitted, when new medications are started and when they’re preparing to leave the ward and venture back out into the wide world. Paediatric pharmacists are also a great source of knowledge around complementary and alternative medicines for children so please discuss any questions you have with them.
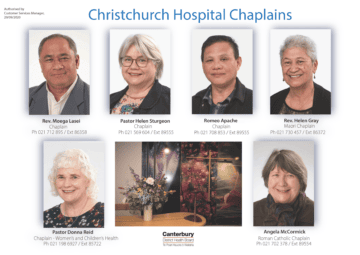
Chaplains
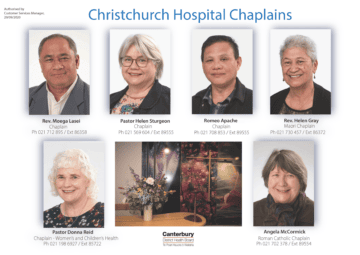
What they do
Chaplains respond to the spiritual, emotional and pastoral needs of patients and their whanau/family. We do this by being a ‘presence’, by listening, affirming other cultures and religions, and by prayers, blessings, encouragement and support. their clinical condition.
When you may see them
Chaplains are available during office hours on-site Monday to Friday, and after hours for emergencies via the operator for the on-call chaplain.
Rev. Moega Lasei
Ph 021 712 895 / Ext 86358
Pastor Helen Sturgeon
Ph 021 569 604 / Ext 89555
Romeo Apache
Ph 021 708 853 / Ext 89555
Pastor Donna Reid Chaplain – Women’s and Children’s Health
Ph 021 198 6927 / Ext 89555
Rev. Helen Gray, Maori Chaplain
Ph 021 730 457 / Ext 86372
Angela McCormick, Roman Catholic Chaplain
Ph 021 702 378 / Ext 89554
Food Services

What they do
Food services is one of the many teams you’ll meet during your stay at Christchurch Hospital. We are fortunate to have passionate assistants like Destiny, who will always take the time to get to know our families.
Not only does Destiny deliver the all-important goodies to our patients, she will check in to make sure our patients are getting exactly what they need – and none of what they don’t if they have allergies or special nutritional requirements. Did you know that fewer than half our patients have ‘set’ meals, so we’re well equipped and ready to make sure patient’s food is prepared especially for them.
Please take the time to introduce yourself to Destiny and her colleagues when they come around to take orders or deliver meals.