Tuesday 7 January 2020Media release4 minutes to read
A new case of measles has been confirmed
Canterbury DHB is alerting the general public that they may have been exposed to measles.
A person has been confirmed as having measles and was infectious while travelling across multiple locations in the South and North Islands between Saturday 28 December 2019 and Monday 6 January 2020.
Canterbury DHB’s Community and Public Health team has been working to identify all close contacts of this person, determining their immunisation status and offering advice regarding what further action they should take.
Anyone who was in the following locations at the times listed should be aware that they may have been exposed and at risk of developing measles, unless they are sure they’ve had two MMR vaccinations or are over 50 years of age. If they are not in either of those two groups, they should isolate themselves at home until the dates listed (inclusive):
- 28 December 2019 – Interislander Ferry Wellington to Picton, 8.45am – 12pm – remain isolated until 11 January 2020
- 30 December 2019 – 03 January 2020 – Whare Flat Folk Music Festival (near Dunedin) – remain isolated until 17 January 2020
- 30-31 December 2019 – ED at Dunedin Hospital between 8.30pm – 1am – remain isolated until 13 January 2020
- 6 January 2020 – Interislander Ferry Picton to Wellington, 2.30–5.45pm – remain isolated until 20 January 2020
Dr Alistair Humphrey, Canterbury Medical Officer of Health, says immunisation is the best protection against measles. This is especially important for children who haven’t yet had their MMR vaccinations scheduled at 15 months and 4 years. These children are currently top priority for vaccination.
“If you are unwell and think it might be measles, stay at home and telephone your General Practice team any time of day or night. Please don’t visit your GP team, other health provider or a hospital in person as this will spread the illness. If it’s an emergency call 111,” says Dr Humphrey. People are considered immune if they have received two doses of MMR vaccine, have already had measles previously, or were born before 1969 – people born before this time will have been exposed to measles and most will therefore have had it.
Dr Humphrey advises that “people are infectious from five days before the onset of the rash until four days after the rash appears, so it is possible to transmit the infection before you feel unwell. People who have been exposed and who are not immune should remain isolated from 7 days after their first exposure to 14 days after their last exposure.”
“This means staying home from school or work and having no contact with unimmunised people. If you are not sure whether you are immune telephone your General Practice team – they can advise you,” says Dr Humphrey.
Anyone with measles symptoms or who believes they may have been exposed, can contact their usual general practice 24/7 for additional advice. If people call their GP Team after hours, they can be put through to a nurse who can provide free health advice and advise what to do and where to go if you need to be seen urgently.
More information about the current measles outbreak is available at https://www.health.govt.nz/your-health/conditions-and-treatments/diseases-and-illnesses/measles/2019-measles-outbreak-information.
ENDS
Measles Fact Sheet
• Measles is a highly infectious viral illness spread by contact with respiratory secretions through coughing and sneezing.
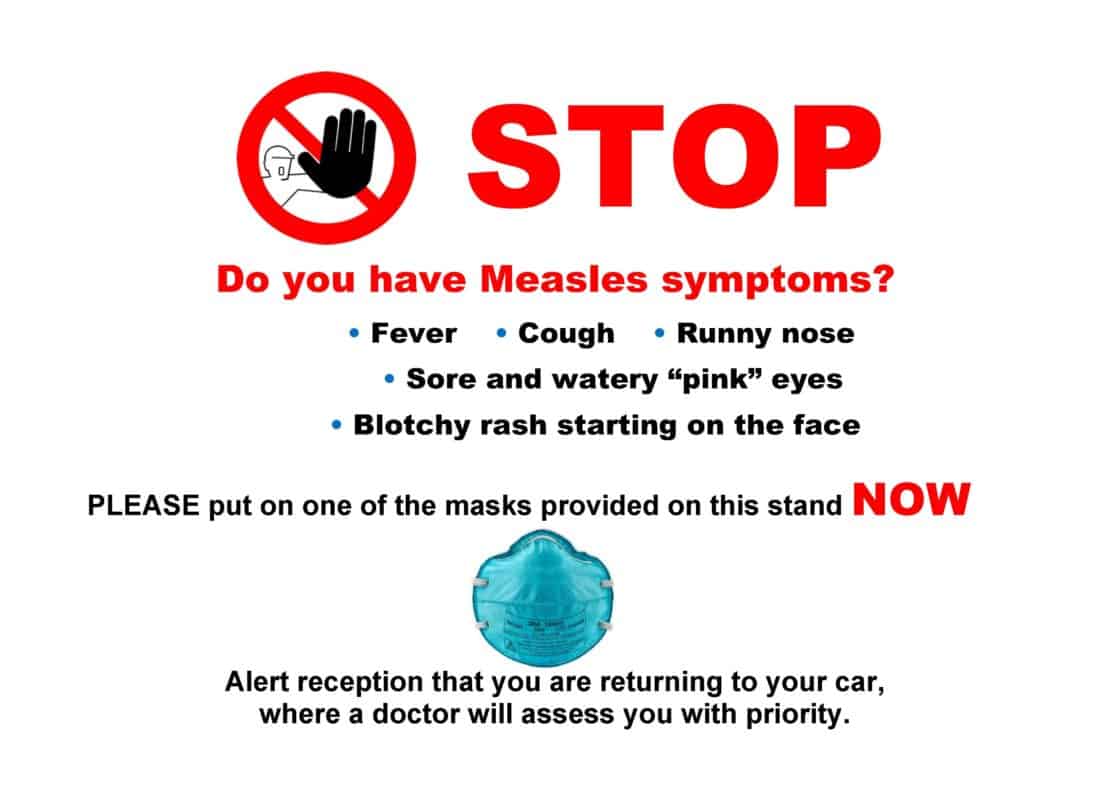
• Symptoms of measles include:
o A respiratory type of illness with dry cough, runny nose, headache.
o Temperature over 38.5 C and feeling very unwell.
o A red blotchy rash starts on day 4-5 of the illness usually on the face and moves to the chest and arms.
• People are infectious from five days before the onset of the rash to four days after the rash starts.
• Infected people should stay in isolation – staying home from school or work – during this time.
• The best protection from measles is to have two MMR vaccinations. MMR is available from your general practice team and is free for eligible people.
• Children and people who have never been immunised are the priorities for the vaccine.
• People are considered immune if they have received two doses of MMR vaccine, have already the measles or were born before 1969.
• Anyone believing they have been exposed to measles or has symptoms, should not go to the ED or after-hours clinic or general practitioner. Instead call your GP any time, 24/7 for free health advice.
Tags MeaslesPublic health
Related topics
Public Health
Back to Health News