My doctor has referred me/my child for a Nuclear Medicine scan, what is the waiting time?
For most scans the waiting time is only 2-6 weeks however, if the scan takes a long time or is more specialised, the waiting time could be longer. Kidney scans following a Urinary Tract Infection are booked months after the UTI according to accepted clinical protocol.
If you are concerned and have not received an appointment within 2 weeks, contact Molecular Imaging to check that we have received a referral from your doctor.
Why do I have 2 scan appointments?
For some scans, the radiopharmaceutical takes time to travel through the body and concentrate in the organ of interest. At the first appointment you will receive an injection and depending on the type of scan, images may also be taken at this time. At the later appointments time/s on the same day, images only will be taken. The exception is a Myocardial Perfusion Rest/Stress scan which has injections at both times.
Do I need to prepare for the scan?
Specific appointment letters are sent out which give details of any special preparations. Please read them carefully. For most scans you can eat and drink normally and keep taking your usual medication.
What if I am pregnant or breastfeeding?
Phone Molecular Imaging. It is usually advisable to delay the scan until after pregnancy unless there is a clinical reason for doing otherwise. Breastfeeding mothers will be given instructions and advice depending on the type of scan they are having, as only some radiopharmaceuticals are excreted in breast milk.
Can I bring a friend, relative or carer with me?
We would welcome this as long as they are not young children or a pregnant woman.
How is the injection given?
A very small needle is used for the injection, which is in a volume of no more than 1ml. A vein in the arm is usually used, although sometimes a hand or foot is more suitable, especially in babies and young children. It will feel similar to a blood test or pin prick. If you have difficulty with blood tests or IV access, please contact Molecular Imaging ASAP.
What is a radiopharmaceutical?
This is a compound which is usually made by mixing a radioactive isotope with a non-radioactive formula. Different compounds are used to study different parts of the body. Over 90% of scans use radioactive 99mTechnetium which has a physical half-life of only 6 hours and an even shorter half-life in the body.
Does the radiopharmaceutical have any side effects?
The injection will not make you feel any different and side effects are very rare. You will NOT glow in the dark!
Is the radiation dangerous?
NO. The radioactivity used has a short life and is quickly eliminated from the body. Even though the radioactivity is injected, most radionuclide scans involve the same amount or less radiation than that from x-ray or CT procedures.
Every possible precaution is taken to minimise the radiation exposure to as small an amount as possible while still obtaining the needed diagnostic information. All babies and children under 18 years old are weighed on arrival and the dose of radioactivity is calculated according to weight.
How long does the radiation take to disappear from the body?
This will depend on the type of scan. In some cases part of the radiation is excreted in the urine and therefore leaves the body quite rapidly.
Radioactive 99mTechnetium decays to a non-radioactive form over a period of 2 days, after 24 hours (4 x half-lives) there will only be very small quantities remaining.
Are there any precautions to follow after the injection?
While we do not consider the radiation emitted a hazard, we have the responsibility to keep radiation exposure to others as low as reasonably achievable.
For some scans, adults are advised to avoid close continuous contact with children and pregnant women for the rest of the day. It is safe to share a bed with your partner on the night of your scan, unless otherwise directed.
Children are advised not to sleep in the same bed as other children and not to go back to school, kindergarten or crèche until the day after the scan. It is preferable to use disposable nappies for the day of the scan and at home normal hygenic measures are sufficient. Remember to wash your hands.
There are no restrictions for handling pets.
What will I need to remove for the scan?
You will not need to remove all your clothing. Usually shoes and metal objects around the area being scanned are all that is necessary, for example you will not need to remove your rings or watch unless the scan is of your hands and wrists. If you have a prosthesis, we may require you to remove it.
You will need to be able to roll up your sleeve to the elbow for the injection. The technologist will tell you exactly what is required before you start your scan.
I have a pacemaker, metal hip/knee/screws/plates, hearing aid. Will this cause a problem with the machine?
NO. It is different altogether from an MRI scans, however please let the scanning staff know if you have a metal implant.
Will I be able to get onto the imaging bed?
The beds are about 40cm wide and hold patients up to 180 kg. Although the beds can be lowered, anyone who is immobilised in a wheelchair will need to be able to transfer themselves across. If you think there may be difficulties please phone the department before the scan.
I am claustrophobic, how close will the camera be?
You will not be enclosed and only certain types of scan will require the camera near the head e.g. bone scans of the whole body or upper body, thyroid, cardiac, lung and brain scans. You will not be left alone, a technologist and friend/ relative can stay close by.
The camera is quiet and you may listen to music or wear eye shades if this helps. You are welcome to bring your iPod, MP3 player to listen to during the scan. Phone the department before the procedure if you wish to discuss your concerns with staff.
How will my child keep still during the scan?
We use velcro bands to keep younger children still during the scan however movement is not totally restricted. The camera has a DVD player attached and we have a limited selection of DVDs for children to watch while they are being scanned, though parents are welcome to bring along any favourites. We also have a limited selection of books and toys.
Distractions such as reading a story, watching a DVD or listening to a music tape are usually effective in reducing movement. You may stay close to your child during the scan. Babies may be more settled if they have the comfort of a pacifier, bottle or toy.
What happens to the results of the scan?
A specialist doctor trained in Nuclear Imaging will report the scan and forward the results electronically to the doctor who requested the scan. In most cases the results are available within 24-48 hours.
The pictures are stored on computer (PACS) which can be accessed by both private and public specialists; if the referring doctor is a GP then a paper copy will be posted.

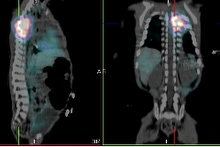
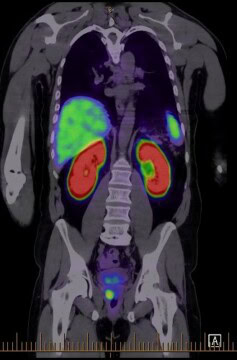
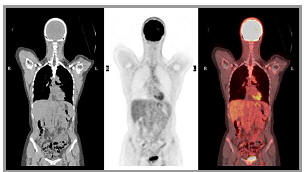 Positron Emission Tomography (PET) is used to demonstrate the metabolic activity of organs and other tissues such as tumours. A radioactive compound called 18FDG (fluorodeoxyglucose) is injected into the patient and the radioactive emissions are measured by a PET/CT scanner. PET is considered particularly effective in identifying whether certain types of cancers are present, if they have spread and if the patient is responding to treatment.
Positron Emission Tomography (PET) is used to demonstrate the metabolic activity of organs and other tissues such as tumours. A radioactive compound called 18FDG (fluorodeoxyglucose) is injected into the patient and the radioactive emissions are measured by a PET/CT scanner. PET is considered particularly effective in identifying whether certain types of cancers are present, if they have spread and if the patient is responding to treatment. use the radioactive element Technetium-99m which is obtained from a small Molybdenum-99 Generator, delivered to the department at the start of each week. Technetium is often mixed with a non-radioactive compound in order to localise the radiopharmaceutical in a specific area in the body.
use the radioactive element Technetium-99m which is obtained from a small Molybdenum-99 Generator, delivered to the department at the start of each week. Technetium is often mixed with a non-radioactive compound in order to localise the radiopharmaceutical in a specific area in the body.


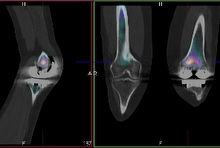
 Bone agents such as HDP localise in regions of increased bone blood flow and increased bone turnover. Almost all significant pathologic processes cause alteration in these physiological parameters, causing increased or occasionally decreased tracer localisation.
Bone agents such as HDP localise in regions of increased bone blood flow and increased bone turnover. Almost all significant pathologic processes cause alteration in these physiological parameters, causing increased or occasionally decreased tracer localisation.  Bone scanning is a well-established technique, and is one of the most reliable, sensitive and valuable procedures in nuclear medicine. The scan can detect abnormalities weeks to months before routine skeletal x-rays. It is particularly useful for assessing patients with pain suspected of bony origin, and evaluating sports injuries. It remains the most cost-effective imaging procedure for assessing skeletal metastatic burden.
Bone scanning is a well-established technique, and is one of the most reliable, sensitive and valuable procedures in nuclear medicine. The scan can detect abnormalities weeks to months before routine skeletal x-rays. It is particularly useful for assessing patients with pain suspected of bony origin, and evaluating sports injuries. It remains the most cost-effective imaging procedure for assessing skeletal metastatic burden.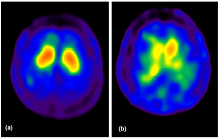 Parkinson's Disease and several other syndromes are characterised by the degeneration of dopaminergic cells, resulting in the loss of Dopamine Transporters (DATs) in the striatum. 99mTc-TroDAT binds to the dopamine transporter, its uptake is significantly reduced in the striatum of patients with Parkinson's Disease.
Parkinson's Disease and several other syndromes are characterised by the degeneration of dopaminergic cells, resulting in the loss of Dopamine Transporters (DATs) in the striatum. 99mTc-TroDAT binds to the dopamine transporter, its uptake is significantly reduced in the striatum of patients with Parkinson's Disease.
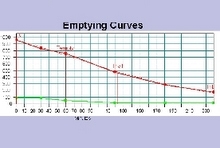 A standard meal of scrambled egg on toast and milk is given to the patient. The egg is pre-labelled with a technetium colloid and the meal is standardised for fat, carbohydrate, protein, and total calorie content.
A standard meal of scrambled egg on toast and milk is given to the patient. The egg is pre-labelled with a technetium colloid and the meal is standardised for fat, carbohydrate, protein, and total calorie content.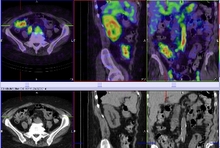 The study should be performed while the patient is actively bleeding. Although the test is sensitive and can detect intermittent bleeding, it may not always localise the exact anatomical site. SPECT/CT can be used to provide anatomical localisation when bleeding is detected.
The study should be performed while the patient is actively bleeding. Although the test is sensitive and can detect intermittent bleeding, it may not always localise the exact anatomical site. SPECT/CT can be used to provide anatomical localisation when bleeding is detected.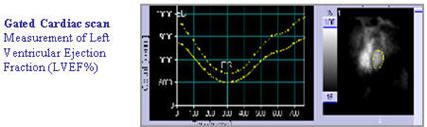
 The radiopharmaceutical 99mTc-Scintimun' used for Infection Imaging,
The radiopharmaceutical 99mTc-Scintimun' used for Infection Imaging,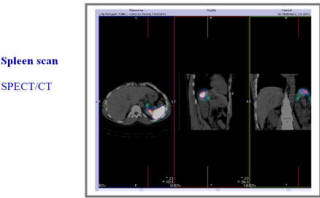 Labelled heat denatured red blood cells are avidly sequestered by the spleen, allowing for selective splenic imaging.
Labelled heat denatured red blood cells are avidly sequestered by the spleen, allowing for selective splenic imaging. -Scan/Lung%20V%20Q%20Scan%20SPECT-CT%20+ve.jpg) Lung VQ scanning should be considered when CTPA is negative or indeterminate and there is a high clinical likelihood, and when there is a contraindication to CTPA (impaired renal function or iodine allergy).
Lung VQ scanning should be considered when CTPA is negative or indeterminate and there is a high clinical likelihood, and when there is a contraindication to CTPA (impaired renal function or iodine allergy).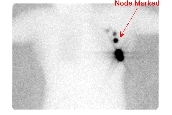 2x 0.1ml of 99mTc-nano-colloid are
2x 0.1ml of 99mTc-nano-colloid are 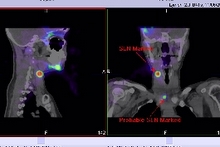 2x 0.1ml of 99mTc-nano-colloid are injected subcutaneously either side of the melanoma or merckle cell scar.
2x 0.1ml of 99mTc-nano-colloid are injected subcutaneously either side of the melanoma or merckle cell scar.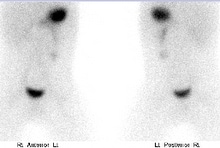
 MIBG sensitivity in the detection of neuroblastoma has been reported to be 90% or greater, specificity approaches 100%. The extent of metastatic bone and bone marrow disease is most accurately defined by MIBG scintigraphy however small liver mets may escape detection due to the high concentration of MIBG in the liver. The accurate depiction of the full extent of disease spread and distribution are essential before therapy for both prognostic classification and therapeutic decisions.
MIBG sensitivity in the detection of neuroblastoma has been reported to be 90% or greater, specificity approaches 100%. The extent of metastatic bone and bone marrow disease is most accurately defined by MIBG scintigraphy however small liver mets may escape detection due to the high concentration of MIBG in the liver. The accurate depiction of the full extent of disease spread and distribution are essential before therapy for both prognostic classification and therapeutic decisions.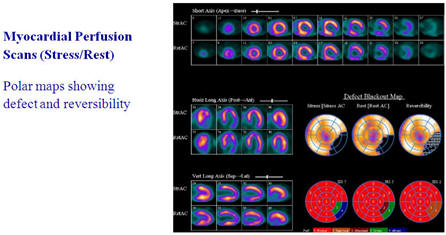
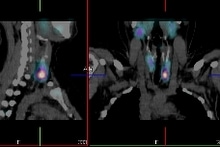
 PSMA is a trans membrane protein with a significantly increased expression in Prostate Cancer cells. The PSMA expression increases progressively with higher grade Prostate Cancer, Prostate Cancer Metastasis and Castrate Resistant Prostate Cancer. 99mTcPSMA can detect recurrent lesions in different locations, such as local recurrence, lymph nodes, bone metastases, and visceral metastases. Detection rate and sensitivity correlate to PSA levels and lesion size.
PSMA is a trans membrane protein with a significantly increased expression in Prostate Cancer cells. The PSMA expression increases progressively with higher grade Prostate Cancer, Prostate Cancer Metastasis and Castrate Resistant Prostate Cancer. 99mTcPSMA can detect recurrent lesions in different locations, such as local recurrence, lymph nodes, bone metastases, and visceral metastases. Detection rate and sensitivity correlate to PSA levels and lesion size. DMSA has a high affinity for proximal tubules and produces superb images of the renal cortex. Renal scanning can readily detect the number, size and position of any functioning kidney. The study is very sensitive in detecting any renal cortical abnormality and exceeds that of an IVU or ultrasound. It is considered the gold standard for screening for cortical scars.
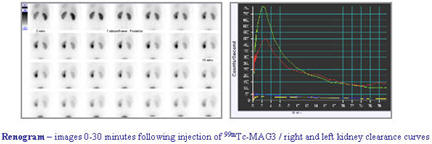
DMSA has a high affinity for proximal tubules and produces superb images of the renal cortex. Renal scanning can readily detect the number, size and position of any functioning kidney. The study is very sensitive in detecting any renal cortical abnormality and exceeds that of an IVU or ultrasound. It is considered the gold standard for screening for cortical scars.