[Video length: 17:15 minutes]
[Title: Swaddled bathing]
[Tiffany Hamilton, Physiotherapist] I’m Tiffany Hamilton. I’m the physiotherapist in the neonatal intensive care unit at Christchurch Women’s Hospital.
I’m very lucky to have wee Tilly with me today, and I’m going to show you how to do swaddle bathing.
It’s a great thing for babies in the neonatal unit to do, um, the environment in the, um, NICU is not what it would normally be for bathing, so this is a lovely way to keep babies calm, give them a feeling of safety and security, and it makes handling really easy.
So I’ve popped two towels on the change table for the baby after the bath.
Um, for swaddling, uh, people swaddle different ways, but I find the best way is take your swaddle, turn down, uh, top corner.
So you’ve got a triangle turned down, which gives you two long arms to wrap your baby in.
And then pop that on your change table on top of your, uh, two towels. And then your bub’s gonna go on the top.
Grab yourself two Muslins, or they could be the, um, soft paper ones as well.
If there aren’t any of these around, obviously you’re going to need all of your baby’s clothes, um, nappy change and something to wipe just in case your baby’s given you a nice surprise of a poo in their nappy.
Here we go.
Yeah. So start with your baby swaddled and then slowly undressing with undressing.
Always roll your baby to the side, tuck them under, and then roll them over their clothes.
Keep their hands to the midline that keeps your baby nice and settled.
Once their hands fling out to the side, they feel a little bit insecure. Take that one over the top.
Yay. The rolling from side to side is really helpful for your baby’s brain development for preterm babies.
If they were still on the inside, they would still be moving around and miss some of that when they’re born early, and they’d have that movement inside with mum moving as well.
So just feed that tube through. If you can pop your baby into sideline, you can see their hands roll forwards to the, to the middle.
Oh, Let’s get these pants off. Okay. Yeah.
Always talk to your baby so they know what’s happening.
Same as you would for a grownup. There we go.
Oh, here we go. Here we go. So you can see Tilly’s fussing a little bit.
She’s telling me, oh, get on with it.
I give her a little bit of support, reassure her ’cause I’m not a mummy, I’m a a stranger in her life.
Yeah. There we go. Sneak you up the bed a little bit.
Always make sure that your swaddle is right there at the top of your baby’s shoulders.
Hands to the middle. One cross little bit of a roll, other hand to the middle, and a little bit of a roll again.
You can see that helps her instantly get her hand into her mouth.
Okay, it’s coming up to food time and she can self-soothe now for washing.
Wet one of your Muslins, and you’re gonna start at the top and work downwards.
That feels better already, doesn’t it? You can see how she settled there just from being swaddled.
So there we go.
Clean behind their ears, that’s can drop their head back a little bit to clean out all that cheesy stuff under your chin.
Got beautiful double chins. Now she says, oh, I just wanna get in the bath now.
It’s okay. Take one side out of the swaddle and do a one arm
Another Side out. Oh, don’t you pull your tube, that’s a girl.
So undo that nappy. Wrap that swaddle again.
Roll and tuck in under the hip every time you do that.
Rolling. It’s great for the development of that part of the brain, the vestibular system, which later down the track, Ms. Tilly’s gonna help with balance.
I’m gonna wash round the join, get rid of that.
Muslin, pop a new one in the bath, and then I’ve got you right where
I need you, up to me. Ready? Ready, ready, ready. Sh.
And hold that over. Hold your baby like a rugby ball. Oh, sh.
Oh, is that better? So one hand at the back and one hand at the front.
Things that your baby feels cocooned, nice and safe.
A swaddle helps bring their hands to the midline, which again helps them with that regulation.
And you can see once you got over that change of sensory environment into a nice warm bath, her eyes are brightened up and she’s listening to me.
She’s looking around. Oh, You all good there? So this is a lovely time.
You’ve done your washing of your baby on the change mat.
So this is a lovely time to engage with your baby.
Have a chat. You can do some singing if you want to.
Singing is great for early brother.
See, I took my hand away and instantly her hands splayed out.
So she’s saying, oh, actually, I liked that, I liked that extra support.
If your baby is a little unsettled in the bath, what you can do is bring them right across to the side of the bath, either close to you, or if you’ve got longer arms than I do over the other side of the bath.
And that extra boundary helps them feel happy. Or you can also make sure their feet are on the end of the bath so they can feel that boundary.
All of these boundaries. So the boundary of the cocoon, the end of the bath of the swaddle feels like a cocoon.
The end of the bath is all similar to what the boundaries of the womb feel like for your baby, and that’s what their brain is expecting as it develops.
How’s that? So again, I’m just gonna take my hands away, see what Tilly does, which is a little more relaxed now.
And I’m gonna take one side of the swaddle off and we’ll see what happens.
Hi. So that yawn is just saying to me, oh, she’s might be getting a little bit tired.
See this arm’s coming out and her hands a splain.
That’s suggesting to me that that might just be a little bit too much for her.
She likes this position tucked in here, and she can get her hands to her mouth and her hands to her face
And, Oh, have you had enough? That’s, I think it’s nearly food time.
So I am going to slowly unwrap her because that’s gonna change her environment.
And then hold onto that shoulder. That’s to the opposite of where I am. Okay.
And then I’ve got full support of her control of her movement.
Then I’m going to slowly unwrap this side and then bring her hands to the middle.
Make sure I’ve got rid of the swaddle.
That’s again, I think we’ll get rid of these. Oh no, they’re not much fun, are they?
You can see the difference for her in the above with and without the Muslin on.
Hi. So I’m gonna bring her hands to the middle.
That’s her safe space and bring her out on her tummy
And Straight onto her side. Is it you, oh yeah. That’s a girl that’s dry off.
So on her side, her hands go straight into her mouth. Ooh.
Just sat straight on her thumb and dry her off.
We’ll Get rid of those old clothes.
Deal with those ones in a minute. It, yeah.
That sideline position is the most soothing for your baby.
If you lie them straight on their back, that’s when they end up like a starfish and get themselves more upset.
Okay. I think you’re pretty hungry. Would you like this?
Oh, yes, please. Oh, yes, please. So do that initial dry off and then
That’s okay. Pardon you.
That’s all those creases I’m gonna pop a nappy on because I’m not that silly to leave one off for too long.
Sideline is a lovely position to pop a nappy on you.
If you find that your baby doesn’t like having a nappy changed, try changing sideline.
Yeah, It’s nearly that time. It’s nearly that
Time. There we go.
Let’s pop your suit on.
So she does a beautiful job of sorting herself out in her environment.
She’s l to bring her hands to her face to self-soothe again.
Roll your baby right over.
Tuck those clothes in here, and then hands to the middle.
Roll Over the top.
Good. Oh yeah. Okay. That’s okay.
I will just borrow that one for a second.
That’s okay. There we go. You are hungry, hungry, hungry, hungry.
Yeah. Are you talking? There we go.
You can see that the speed of handling is really important for your baby.
Slow and predictable is really important for preterm infants.
Okay. Anytime there where I’ve gone a little bit fast, or I haven’t supported her.
When I’ve moved her, she’s become unhappy with me.
And that’s because I haven’t gone slowly enough for her.
Okay. I’m gonna bend that one up. Yeah. So one side in first hands to the middle, roll your baby over.
There we go. And as you are rolling over, you can give them some nice firm holding.
And again, that helps with that feeling of security.
With that deep touch, a little bit of firm pressure, particularly for babies from about 36 weeks onwards, is really lovely for the sensory system.
Touch is the first system to develop for a baby.
And so it’s one of the most important that we look after.
I know you just wanna have something to eat, don’t you?
This one’s too small, Ms Tilly, but we’re gonna run with it.
Hungry. Twinkle. Twinkle little star, how I wonder what you are. You’re a thinker.
Singing to your baby is one of the loveliest ways to develop their brains, as is reading.
But singing’s really simple. Just share those songs that you grew up with. And changing time is a perfect time to do that. Okay.
Oh, So there we go. All clean, washed. Ready to go? Yeah.
So thank you Tilly. Thank you to your mommy for lending you to me and to your sister Ivy.
Lovely. Thanks a lot.
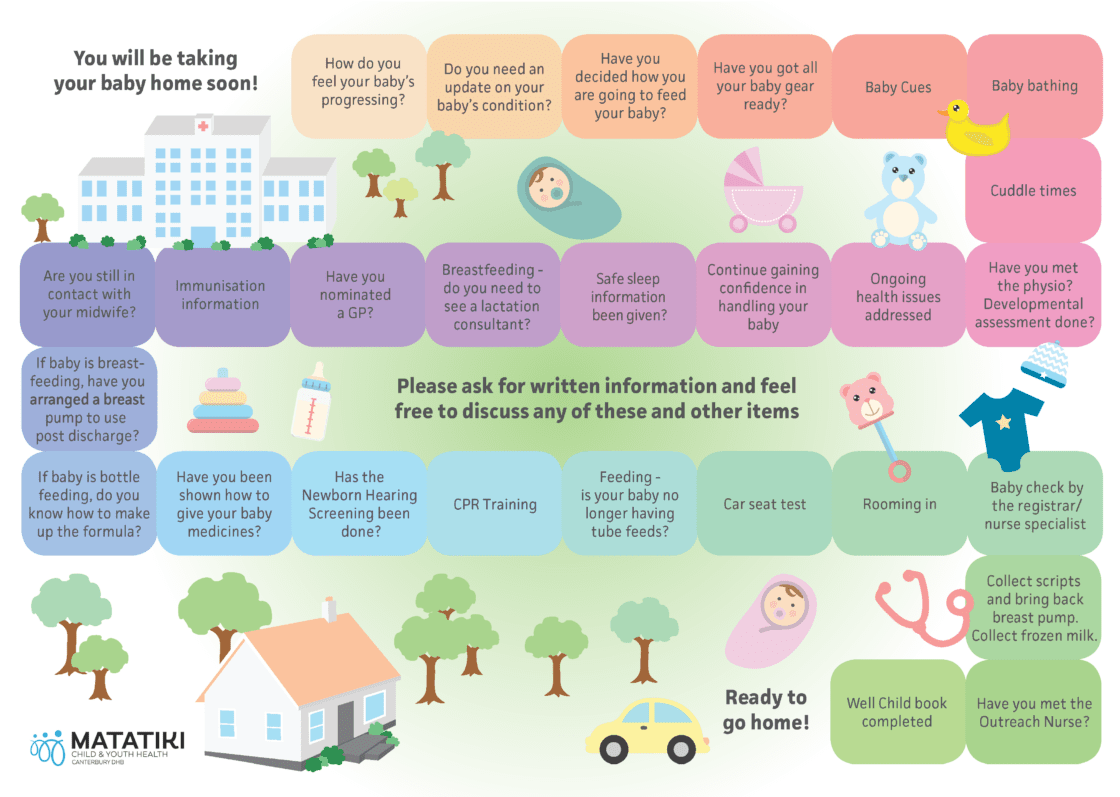
[Credits: Remember: Get everything ready before the bath, so that you can be present with your baby.
Swadling keeps your baby calm and focused it helps them feel safe and secure, conserving energy for feeding and growing.
Talking and singing to your baby helps build their brain – perfect at bath time.
Give firm, secure touch with movement to help early brain development. Keep hands to the midline and use rolling.
Watch your baby’s face and body movements – they will let you know what they need and when they’ve had enough.
Ask your nurse for an education sheet for Swaddled bathing.]